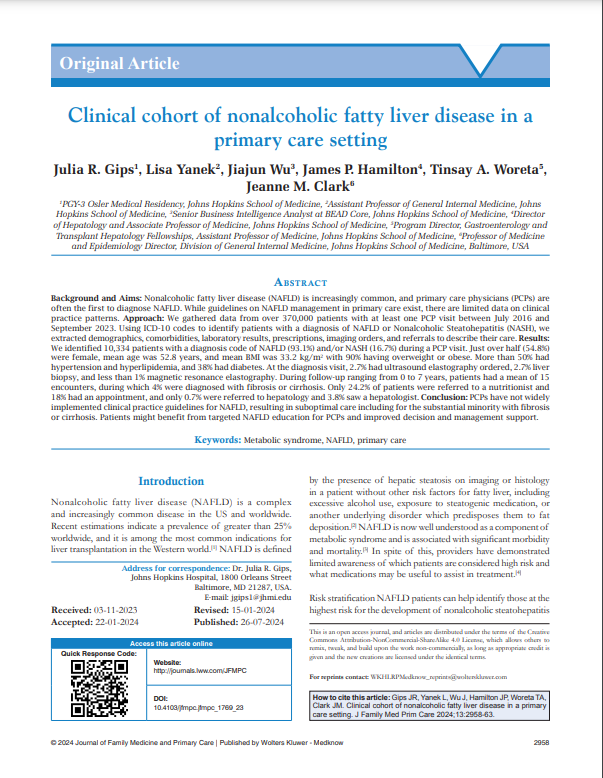
Clinical cohort of nonalcoholic fatty liver disease in a primary care setting
August 2024
Journal of Family Medicine and Primary Care
Abstract
Background and Aims:
Nonalcoholic fatty liver disease (NAFLD) is increasingly common, and primary care physicians (PCPs) are often the first to diagnose NAFLD. While guidelines on NAFLD management in primary care exist, there are limited data on clinical practice patterns.
Approach:
We gathered data from over 370,000 patients with at least one PCP visit between July 2016 and September 2023. Using ICD-10 codes to identify patients with a diagnosis of NAFLD or Nonalcoholic Steatohepatitis (NASH), we extracted demographics, comorbidities, laboratory results, prescriptions, imaging orders, and referrals to describe their care.
Results:
We identified 10,334 patients with a diagnosis code of NAFLD (93.1%) and/or NASH (16.7%) during a PCP visit. Just over half (54.8%) were female, mean age was 52.8 years, and mean BMI was 33.2 kg/m2 with 90% having overweight or obese. More than 50% had hypertension and hyperlipidemia, and 38% had diabetes. At the diagnosis visit, 2.7% had ultrasound elastography ordered, 2.7% liver biopsy, and less than 1% magnetic resonance elastography. During follow-up ranging from 0 to 7 years, patients had a mean of 15 encounters, during which 4% were diagnosed with fibrosis or cirrhosis. Only 24.2% of patients were referred to a nutritionist and 18% had an appointment, and only 0.7% were referred to hepatology and 3.8% saw a hepatologist.
Conclusion:
PCPs have not widely implemented clinical practice guidelines for NAFLD, resulting in suboptimal care including for the substantial minority with fibrosis or cirrhosis. Patients might benefit from targeted NAFLD education for PCPs and improved decision and management support.